In resolution of diabetes, MGB showed spectacular results: 94.4% stopped diabetic medications a few weeks after MGB, 76.2% after RYGB and 59.4% after LSG.
BARIATRIC Surgeon, Gurvinder S Jammu and nutritionist/dietitian Rajni Sharma, MSc, audited 1,107 cases, comparing SG, RYGB and MGB, at the Jammu Hospital, Jalandhar, state of Punjab in Northwest India to find MGB Out Performs SG and RYGB
Their seven-year data (Jan 2007 to Mar 2014) was collected prospectively and reviewed retrospectively, with a database of 473 MGBs, 339 LSGs, and 295 RYGBs.
The study, ‘A 7-Year Clinical Audit of 1107 Cases Comparing Sleeve Gastrectomy, Roux-En-Y Gastric Bypass, and Mini-Gastric Bypass, to Determine an Effective and Safe Bariatric and Metabolic Procedure’, was reported in Obesity Surgery (online first). India is known for prevalence of undernutrition, but a significant obese population co-exists.
Punjab is one of the most obese states in India with incidence 33.8%. Impaired glucose tolerance with metabolic syndrome has frequent onset in South-east Asians at BMI >22.
Patients were assessed for nutritional status, medical fitness and psychological well-being by the bariatric surgeon, physician, anesthetist, and bariatric counselor.
Patients were presented with three options in detail – LSG, RYGB and MGB after one-on-one consultations with surgeon and medical team.
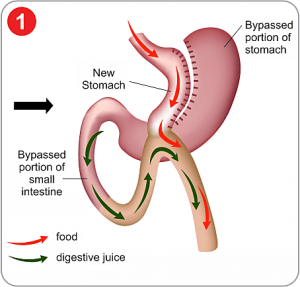
Written informed consent was obtained from all patients. MGB used the Rutledge technique with first stapler firing perpendicular to lesser curvature distal to crow’s foot, followed by vertical gastric division proximally to the left of the angle of His (which was not dissected).
Next, jejunum was measured to 200cm distal to Treitz’ ligament, where a wide antecolic gastrojejunostomy was performed (leading to low intraluminal pressure).
LSG was started by dissecting across antrum 3-5cm proximal to pylorus. Laparoscopic RYGB created a 30-50 ml gastric pouch to the lesser curvature, with the jejunum transected 50cm distal to Treitz’ ligament, with the proximal divided end of jejunum anastomosed 75cm distally, where a side-to-side entero-enteral anastomosis was done. For %EWL and resolution of co-morbidities, only patients with mean follow-up of 53.5 months (20-87 months) made up the patient material.
Follow-up was by monthly visits, phone calls and email. Data included outcomes at 30 days, three months, six months, one year, and yearly thereafter.
All patients signed a declaration that they will stay in contact throughout life, either in person/phone/email.
Follow-up was first year 94.7%, second year 90.8%, third year 81.4%, fourth 75.1%, fifth 72.2%, sixth 68.9%, and seventh year 52.7%.
The three operative groups were demographically comparable in age, sex and weight. Mean operating time was 60.0mins for LSG, 160.5mins for RYGB and 57.5mins for MSG.
Mortality was 2.1% in LSG, 0.3% in RYGB, and zero in MGB. Leaks were highest in LSG (1.5%), followed by RYGB (0.3%) and zero in MGB.
One patient after LSG had persistent vomiting which progressed to Wernicke’s encephalopathy.
Bile reflux was seen transiently in 0.4% after MGB. GERD occurred in 9.4% after LSG, 1.7% after RYGB, and 0.6% after MGB.
One patient after RYGB had marginal ulceration (a smoker who improved with conservative methods).
Three patients after MGB had marginal ulcer, and all responded to conservative management – PPI, yoghurt and cessation of cigarettes, NSAIDs and alcohol.
One patient after RYGB had persistent vomiting one year post-op, which responded to endoscopic dilatation of a stenosis.
There was no internal hernia after LSG and MGB but it occurred in 2.0% after RYGB. Resolution of type 2 diabetes, dyslipidemia, and hypertension was maximal in MGB.
In resolution of diabetes, MGB showed spectacular results: 94.4% stopped diabetic medications a few weeks after MGB, 76.2% after RYGB and 59.4% after LSG.
The Jammu Hospital in Jalandhar has a comprehensive dedicated laparoscopic and bariatric surgery programme Hypoalbuminemia was minimal in LSG and 2.0% in RYGB.
However, after MGB, 13.1% had hypoalbuminemia which was severe in 3.8% (250cm (two required reversal), but not subsequently where a maximum of 230-250cm was bypassed and small bowel was run to ensure that >300cm was maintained distally. Hypoalbuminemia responded to high-protein diet and Creon (pancrelipase).
In all cases of MGB where the length of the bypass was 200cm, no hypoalbuminemia resulted.
Anemia was highest in MGB (4.9%), followed by RYGB (4.8%) and LSG (3.5%), in menstruating women. Proferrin® (iron heme peptide) is taken orally t.i.d. MGB patients had EWL >90%, while EWL was 72% and 53% after RYGB and LSG respectively.
Weight regain occurred in 14.2% after LSG, 8.5% after RYGB. After MGB, weight loss was >75% even after six years, Hair loss was common after all three procedures, but highest after MGB (10.1%), followed by RYGB (8.5%) and LSG (8.0%).
MGB superseded RYGB in technical ease, efficacy, revisability, and reversibility which shows that MGB Out Performs SG and RYGB
With all considered, the authors concluded that MGB is the most effective and safe procedure in patients who are compliant in taking calcium and iron supplements.
LSG may be done in evaluated non-compliant patients who may accept weight regain. On invitation, I addressed the Indian Medical Association, Jalandhar Chapter on bariatric surgery.
I was impressed with the organization and patient care at Jammu Hospital, which has stringent Indian National Accreditation Board standards for 18 specialties, including bariatric and metabolic surgery.
Source : Bariatric News : Bariatric News India
For further/any queries write to Dr GS Jammu (Mini Gastric Bypass Surgeon in India) at: drgsjammu@gmail.com | info@jammuhospital.com
Call at: +91 8283 0000 10 or +91 98140 70870
