Best Laparoscopy Surgery Hospital in Jalandhar Punjab India
Advanced Laparoscopic Surgery Center
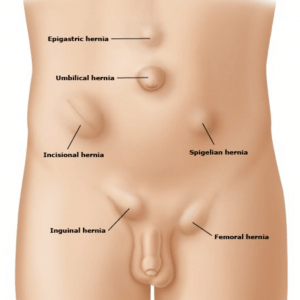
Inguinal Hernia
An inguinal hernia is a common medical condition where tissue, often part of the intestine, protrudes through a weakened area in the abdominal muscles, typically resulting in a visible bulge in the groin. If left untreated, it can lead to discomfort, pain, or complications. Causes include weakened abdominal muscles due to factors like aging, strenuous activity, chronic coughing, or conditions increasing intra-abdominal pressure.
In men, inguinal hernias commonly develop in the inguinal canal, through which the spermatic cord passes from the abdomen to the scrotum. In women, they can occur in the inguinal canal or the area where the round ligament of the uterus passes through the abdominal wall.
Symptoms often include a noticeable bulge in the groin area, which may worsen with activities like standing, coughing, or straining. Discomfort, pain, or a feeling of heaviness can also occur. In severe cases, complications like incarceration or strangulation may arise, leading to emergency situations due to trapped or compromised blood supply to the herniated tissue.
Diagnosis typically involves a physical examination by a healthcare professional, where the bulge may be observed or felt. Imaging tests such as ultrasound or MRI may be used to confirm the diagnosis or assess the extent of the hernia.
Treatment usually involves surgical repair to strengthen the weakened abdominal wall and reposition the tissue. Surgery may be performed through open or minimally invasive techniques like laparoscopy, depending on the hernia’s size and severity. In some instances, a watchful waiting approach may be recommended for asymptomatic or minimally symptomatic hernias, particularly in individuals with health issues making surgery risky.
Early detection and timely treatment are crucial to prevent complications and improve outcomes. Individuals with symptoms suggestive of an inguinal hernia should seek medical attention for proper evaluation and management. Maintaining a healthy weight, avoiding heavy lifting or straining, and addressing conditions increasing intra-abdominal pressure can help reduce the risk of developing inguinal hernias.
Umbilical Hernia
An umbilical hernia is a common condition where a portion of the intestine or abdominal tissue protrudes through a weakened area near the belly button (umbilicus). This type of hernia typically presents as a visible bulge or swelling in the abdominal area around the navel and may vary in size from small to large. Understanding the causes, symptoms, and treatment options for umbilical hernias is essential for effective management and prevention of potential complications.
The development of an umbilical hernia often occurs due to a weakness in the abdominal muscles around the umbilicus. This weakness can be congenital (present from birth) or acquired, resulting from factors such as obesity, pregnancy, abdominal surgery, or increased abdominal pressure due to activities like heavy lifting or chronic coughing. In infants, umbilical hernias are relatively common and may develop as a result of incomplete closure of the abdominal muscles around the umbilical cord after birth.
Symptoms of an umbilical hernia typically include a visible bulge or swelling near the belly button, which may become more noticeable when coughing, straining, or standing upright. In some cases, the bulge may disappear when lying down or gently pushing it back into place. Most umbilical hernias are not associated with significant pain or discomfort, although larger hernias or those that become incarcerated (trapped) may cause discomfort or complications such as strangulation (restriction of blood flow to the herniated tissue).
Diagnosis of an umbilical hernia usually involves a physical examination by a healthcare professional, during which the characteristic bulge may be observed or palpated. In some cases, imaging tests such as ultrasound or MRI may be ordered to confirm the diagnosis or evaluate the extent of the hernia, particularly if complications are suspected.
Treatment options for umbilical hernias depend on factors such as the size of the hernia, symptoms, and the individual’s overall health. In infants with small, asymptomatic umbilical hernias, watchful waiting may be recommended, as many hernias close on their own by the age of 2 or 3 without intervention. However, if the hernia persists beyond early childhood or causes significant symptoms, surgical repair may be necessary to close the defect in the abdominal wall and prevent complications.
In adults, umbilical hernias are typically repaired surgically, either through open or minimally invasive techniques such as laparoscopy. Surgical repair aims to strengthen the weakened abdominal muscles and reposition the protruding tissue to reduce the risk of recurrence and complications.
Maintaining a healthy weight, avoiding activities that increase abdominal pressure, and addressing underlying conditions such as obesity or chronic coughing can help reduce the risk of developing umbilical hernias. Individuals experiencing symptoms suggestive of an umbilical hernia should seek medical attention for proper evaluation and management. Early detection and prompt treatment of umbilical hernias are essential to prevent complications and improve outcomes.
Femoral Hernia
A femoral hernia is a type of hernia that occurs when abdominal tissue, usually part of the intestine, protrudes through a weak spot in the groin or upper thigh region. Unlike inguinal hernias, which typically occur in the inguinal canal, femoral hernias develop lower down in the femoral canal, a passageway near the groin where blood vessels and nerves travel from the abdomen to the leg. Understanding the causes, symptoms, and treatment options for femoral hernias is essential for effective management and prevention of potential complications.
The development of a femoral hernia often occurs due to a weakness in the abdominal wall or the femoral canal, which can be congenital (present from birth) or acquired. Risk factors for femoral hernias include female gender, older age, obesity, pregnancy, chronic constipation, and conditions that increase intra-abdominal pressure such as heavy lifting or straining. Femoral hernias are more common in women than in men, with the majority occurring in individuals over the age of 50.
Symptoms of a femoral hernia typically include a visible bulge or swelling in the groin or upper thigh area, which may become more prominent when standing, coughing, or straining. Unlike inguinal hernias, femoral hernias often present as a small, firm lump that may be tender to the touch. In some cases, the hernia may cause discomfort or pain, particularly if the protruding tissue becomes incarcerated (trapped) or strangulated (compromised blood supply).
Diagnosis of a femoral hernia usually involves a physical examination by a healthcare professional, during which the characteristic bulge may be observed or felt. Imaging tests such as ultrasound or MRI may be ordered to confirm the diagnosis or evaluate the extent of the hernia, particularly if complications are suspected.
Treatment options for femoral hernias typically involve surgical repair to strengthen the weakened abdominal wall and reposition the protruding tissue. Surgical repair aims to close the defect in the femoral canal and reduce the risk of recurrence and complications such as incarceration or strangulation. Depending on the size and severity of the hernia, surgery may be performed using open or minimally invasive techniques such as laparoscopy.
Early detection and prompt treatment of femoral hernias are essential to prevent complications and improve outcomes. Individuals experiencing symptoms suggestive of a femoral hernia should seek medical attention for proper evaluation and management. Maintaining a healthy weight, avoiding activities that increase intra-abdominal pressure, and addressing underlying conditions such as obesity or chronic constipation can help reduce the risk of developing femoral hernias.
Hiatal Hernia
A hiatal hernia is a condition where part of the stomach protrudes upward through the diaphragm into the chest cavity. The diaphragm, a large muscle that aids in breathing, normally has an opening called the hiatus through which the esophagus passes to connect to the stomach. However, in cases of hiatal hernia, this opening becomes enlarged or weakened, allowing a portion of the stomach to push through.
There are two main types of hiatal hernias: sliding hernias and paraesophageal hernias. Sliding hernias are the most common type, where the junction between the esophagus and stomach, known as the gastroesophageal junction, and a portion of the stomach slide upward into the chest. This type is often associated with gastroesophageal reflux disease (GERD), as the displacement of the stomach can lead to the reflux of stomach acid into the esophagus, causing symptoms like heartburn, regurgitation, and difficulty swallowing.
Paraesophageal hernias, on the other hand, involve a portion of the stomach pushing through the hiatus alongside the esophagus, without disrupting the gastroesophageal junction’s normal position. While less common than sliding hernias, paraesophageal hernias can be more severe as they may lead to complications such as obstruction or strangulation of the stomach, which requires immediate medical attention.
The exact cause of hiatal hernias is not always clear, but risk factors include age (as the muscles supporting the diaphragm may weaken over time), obesity, pregnancy, persistent coughing or vomiting, and frequent lifting of heavy objects.
Diagnosis of hiatal hernias typically involves a combination of medical history, physical examination, and imaging tests such as X-rays or endoscopy. Treatment options range from lifestyle modifications and medications to surgery in severe cases. Lifestyle changes may include weight loss, avoiding large meals, quitting smoking, and elevating the head of the bed while sleeping to reduce reflux symptoms. Medications like antacids, proton pump inhibitors, or H2-receptor antagonists can help alleviate acid reflux. In cases where conservative measures fail or complications arise, surgical repair of the hernia may be necessary to reposition the stomach and close the opening in the diaphragm. Overall, early diagnosis and management of hiatal hernias are essential in preventing complications and improving quality of life.
Epigastric Hernia
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Incisional Hernia
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Inguinal Hernia
An inguinal hernia is a common medical condition characterized by the protrusion of tissue, usually a part of the intestine, through a weakened area or opening in the abdominal muscles. This type of hernia typically manifests as a visible bulge in the groin area and can lead to discomfort, pain, or other complications if left untreated. Understanding the causes, symptoms, and treatment options for inguinal hernias is crucial for effective management and prevention of potential complications.
The most common cause of inguinal hernias is weakness in the abdominal muscles, which can occur due to various factors such as aging, strenuous physical activity, chronic coughing, or conditions that increase intra-abdominal pressure. In men, inguinal hernias often develop in the inguinal canal, a passage through which the spermatic cord passes from the abdomen to the scrotum. In women, they can occur in the inguinal canal or the area where the round ligament of the uterus passes through the abdominal wall.
Symptoms of an inguinal hernia typically include a noticeable bulge in the groin area, which may become more prominent when standing, coughing, or straining. Some individuals may also experience discomfort, pain, or a feeling of heaviness in the affected area. In some cases, inguinal hernias may lead to complications such as incarceration (when the protruding tissue becomes trapped and unable to return to its normal position) or strangulation (when the blood supply to the herniated tissue is compromised).
Diagnosis of an inguinal hernia usually involves a physical examination by a healthcare professional, during which the characteristic bulge may be observed or felt. Imaging tests such as ultrasound or MRI may be ordered to confirm the diagnosis or evaluate the extent of the hernia.
Treatment options for inguinal hernias typically involve surgical repair to strengthen the weakened abdominal wall and reposition the protruding tissue. Depending on the size and severity of the hernia, surgery may be performed using open or minimally invasive techniques such as laparoscopy. In some cases, a watchful waiting approach may be recommended for asymptomatic or minimally symptomatic hernias, particularly in individuals with underlying health issues that make surgery risky.
Early detection and prompt treatment of inguinal hernias are essential to prevent complications and improve outcomes. Individuals experiencing symptoms suggestive of an inguinal hernia should seek medical attention for proper evaluation and management. Additionally, maintaining a healthy weight, avoiding heavy lifting or straining, and addressing conditions that increase intra-abdominal pressure can help reduce the risk of developing inguinal hernias.
Umbilical Hernia
An umbilical hernia is a common condition where a portion of the intestine or abdominal tissue protrudes through a weakened area near the belly button (umbilicus). This type of hernia typically presents as a visible bulge or swelling in the abdominal area around the navel and may vary in size from small to large. Understanding the causes, symptoms, and treatment options for umbilical hernias is essential for effective management and prevention of potential complications.
The development of an umbilical hernia often occurs due to a weakness in the abdominal muscles around the umbilicus. This weakness can be congenital (present from birth) or acquired, resulting from factors such as obesity, pregnancy, abdominal surgery, or increased abdominal pressure due to activities like heavy lifting or chronic coughing. In infants, umbilical hernias are relatively common and may develop as a result of incomplete closure of the abdominal muscles around the umbilical cord after birth.
Symptoms of an umbilical hernia typically include a visible bulge or swelling near the belly button, which may become more noticeable when coughing, straining, or standing upright. In some cases, the bulge may disappear when lying down or gently pushing it back into place. Most umbilical hernias are not associated with significant pain or discomfort, although larger hernias or those that become incarcerated (trapped) may cause discomfort or complications such as strangulation (restriction of blood flow to the herniated tissue).
Diagnosis of an umbilical hernia usually involves a physical examination by a healthcare professional, during which the characteristic bulge may be observed or palpated. In some cases, imaging tests such as ultrasound or MRI may be ordered to confirm the diagnosis or evaluate the extent of the hernia, particularly if complications are suspected.
Treatment options for umbilical hernias depend on factors such as the size of the hernia, symptoms, and the individual’s overall health. In infants with small, asymptomatic umbilical hernias, watchful waiting may be recommended, as many hernias close on their own by the age of 2 or 3 without intervention. However, if the hernia persists beyond early childhood or causes significant symptoms, surgical repair may be necessary to close the defect in the abdominal wall and prevent complications.
In adults, umbilical hernias are typically repaired surgically, either through open or minimally invasive techniques such as laparoscopy. Surgical repair aims to strengthen the weakened abdominal muscles and reposition the protruding tissue to reduce the risk of recurrence and complications.
Maintaining a healthy weight, avoiding activities that increase abdominal pressure, and addressing underlying conditions such as obesity or chronic coughing can help reduce the risk of developing umbilical hernias. Individuals experiencing symptoms suggestive of an umbilical hernia should seek medical attention for proper evaluation and management. Early detection and prompt treatment of umbilical hernias are essential to prevent complications and improve outcomes.
Femoral Hernia
A femoral hernia occurs when tissue protrudes through the femoral canal in the upper thigh, below the groin, more commonly affecting women. Symptoms include a lump in the thigh or groin that intensifies with standing or lifting, and possibly pain. This condition can lead to severe complications, such as infection or bowel obstruction, if the herniated tissue becomes trapped. Diagnosis is through physical examination and may include imaging tests. Treatment generally involves surgery, either open or laparoscopic, to repair the hernia. Preventive measures include maintaining a healthy weight, avoiding heavy lifting, and managing chronic cough or constipation. Prompt medical consultation is advised for those experiencing symptoms.
Hiatal Hernia
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Epigastric Hernia
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
Incisional Hernia
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.
For more information or Booking an Appointment.
Call : +91 99143 70870
Visit our Laparocopy Youtube Channel
[ Jammu Hospital, Laparoscopy & Laser Surgery Center ]
Dr. Gurvinder Singh Jammu opened Jammu Hospital in 2004, where he practiced most advanced surgeries.
Jammu Hospital started as 10 bedded hospital in 2000 at an old building but with increasing popularity and good outcome prompted to shift the hospital in a new building with 43 beds.
Jammu Hospital became a Multi Super Specialty Hospital, serving patients with multiple specialties.
Jammu Hospital is accredited with highest National & International Accreditations: NABH (National Accreditation Board of Hospitals and Healthcare Providers)
& IEF (International Excellence Federation for Metabolic & Bariatric Surgery).
This center is performing the highest number of successful bariatric/weight loss/mini gastric bypass procedures in India.
Jammu Hospital Jalandhar is the only non-corporate hospital in India to have three fully integrated OR1 (Karl Storz Germany) Operating Rooms.
Thus, making the operating rooms world-class, infection-free, non-obstructive workflow & live streaming ready.
Best Laparoscopy Surgery Hospital in Jalandhar Punjab
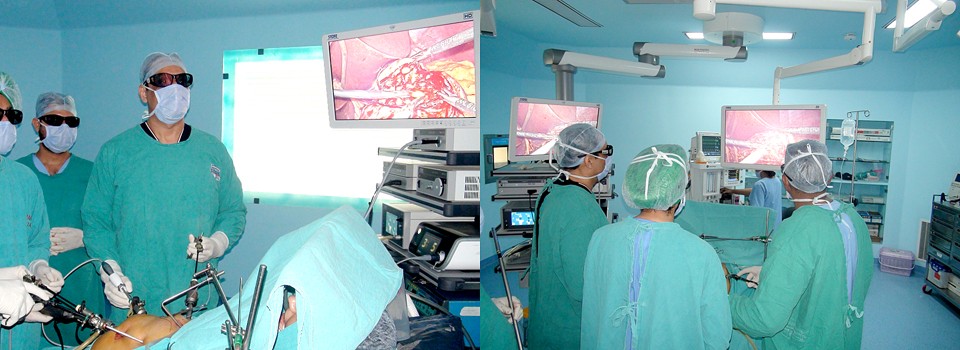

The present era is the era of minimally invasive surgery. At Jammu Hospital we perform all types of Advance & Routine Laparoscopic Surgeries e.g. for Gallbladder Stone, Appendix, Ovarian cyst, Diagnostic laparoscopies, etc.
For more information or Booking an Appointment.
Call : +91 99143 70870